In May of this year, Array was asked to join an Integrated Project Delivery (IPD) team on a complex project with a major healthcare provider in New York City to renovate a fully operational outpatient center in an area of the City undergoing rapid demographic and socioeconomic change. The leadership team wants to create a healthcare environment that is designed with the patient at the center supported by lean principles both in work process and the physical space. Although the project was already underway, the client’s internal Lean director sought Array’s expertise due to our process-led approach they experienced on another current project.
Within a week of being asked to join the project, I accompanied the client leadership team (comprised of administrators, an internal lean team, IT leaders and physicians) at a three-day workshop at the Virginia Mason Institute in Seattle, Washington. The workshop focused on applying lean principles to flow in ambulatory care environments with the goals of learning all we could, building consensus across the leadership team, and applying relevant principles and tools to the client’s organization and to our project. In addition to the 8am-5pm workshop days, we ran our own work sessions from 7-10pm each night to reflect on what we had learned each day and begin visioning and flow mapping our project. The result of the whirlwind trip was consensus from the group that this new project would be developed with lean principles with incorporation of some of the tools we learned about in Seattle, in particular the flow station and the use of dual access exam rooms connected to off-stage integrated team centers.
 One of the greatest challenges for care teams and health systems today is providing truly patient focused, collaborative care in a time where indirect care, digital documentation in an EHR, emails, MD signatures, lab results and appointment scheduling, is growing at a similar rate to the expectations of patients to have on-demand care and information. Virginia Mason’s strategy for working in this new landscape is to keep teams working “in flow.” In ambulatory care, a key example of this is a physician/provider and a medical assistant (MA). This paring of the traditional approach is somewhat upended by putting more power in the hands of the MA than is common to organize and facilitate the indirect care work such that the provider can attend to it incrementally through the day instead of in a pile at the end of a night or, even worse, a week. By keeping a finger on the pulse of the patient load and the indirect care load, the MA keeps the flow of patients steady while helping the provider stay on track with both the face-to-face interactions and the just as critical indirect care.
One of the greatest challenges for care teams and health systems today is providing truly patient focused, collaborative care in a time where indirect care, digital documentation in an EHR, emails, MD signatures, lab results and appointment scheduling, is growing at a similar rate to the expectations of patients to have on-demand care and information. Virginia Mason’s strategy for working in this new landscape is to keep teams working “in flow.” In ambulatory care, a key example of this is a physician/provider and a medical assistant (MA). This paring of the traditional approach is somewhat upended by putting more power in the hands of the MA than is common to organize and facilitate the indirect care work such that the provider can attend to it incrementally through the day instead of in a pile at the end of a night or, even worse, a week. By keeping a finger on the pulse of the patient load and the indirect care load, the MA keeps the flow of patients steady while helping the provider stay on track with both the face-to-face interactions and the just as critical indirect care.
This teaming principle is based on the Lean concept of the work cell. A work cell is made of a group of people with complementary skill sets who work toward the common goal of patient satisfaction and zero defect care. By aligning skill sets to tasks, the work cell allows each individual to work to their fullest potential and abilities. This also creates a culture of mentoring relationships between providers and MAs.
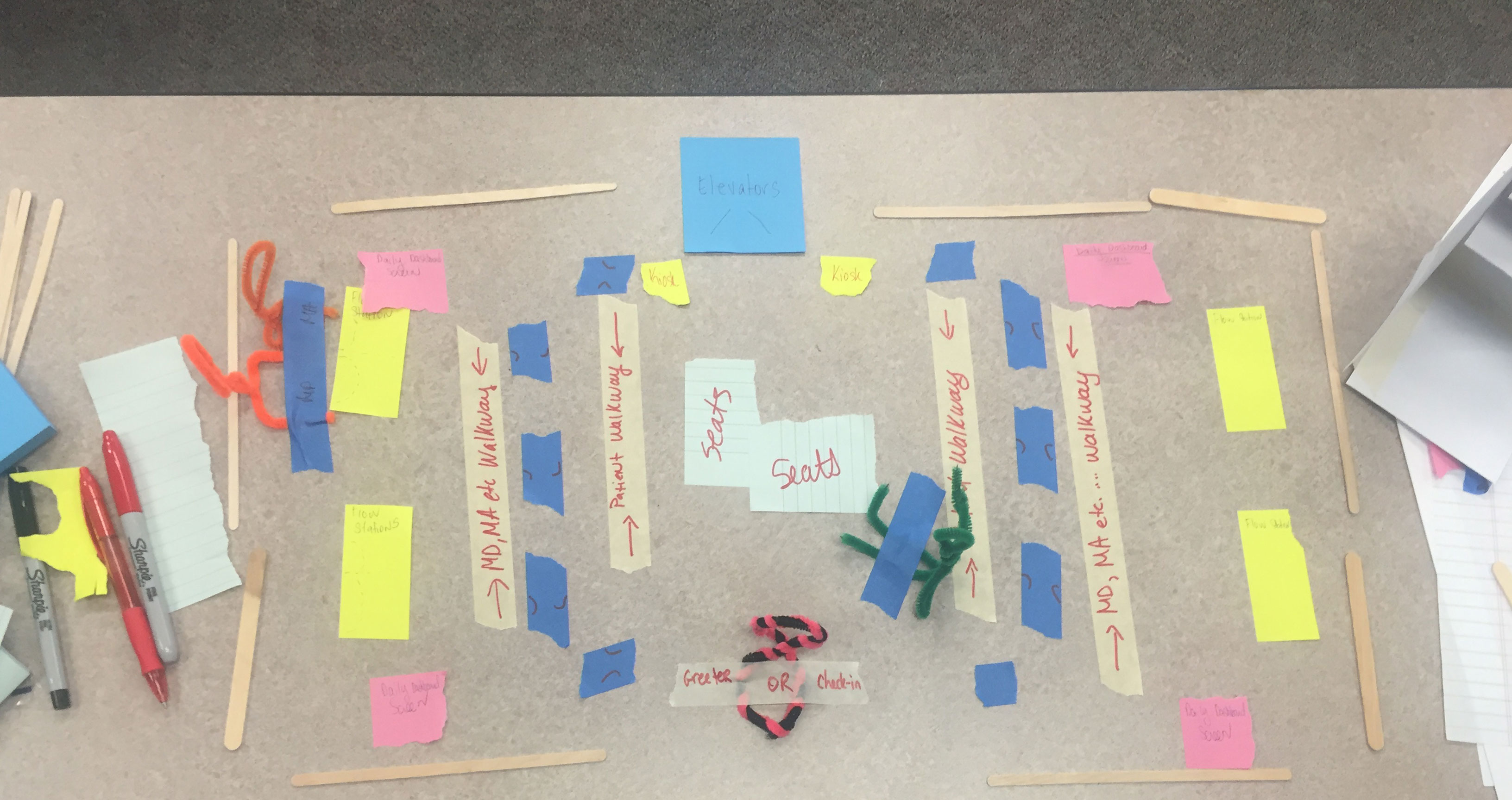
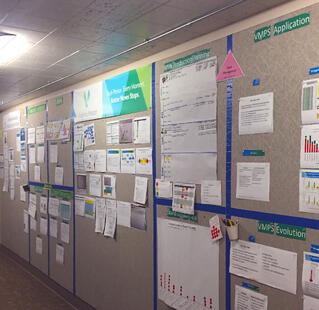
The physical manifestation of the provider/flow manager team is the Flow Station. This is a simple but elegant intervention that facilitates the standard work process developed by the dyad. It provides a computer for each provider and flow manager, with space between to prioritize and review any paperwork that may not be in the digital system. In our client’s case, there is still enough paper flow that in-boxes are needed. As we work with this client, who is about to launch a fully integrated EHR including scheduling and billing, we may find their systems are robust enough to need less paper space.
 In many cases, dual access exam room with an off-stage team center creates too much circulation space in a design – especially on large floor
In many cases, dual access exam room with an off-stage team center creates too much circulation space in a design – especially on large floor
plans. In the case of our project, we’ve been able to make the constraints of the building work in our favor. By placing staff work areas on the building perimeter, the work cell will have access to natural light close to the exam rooms it serves. The work areas are designed to include storage for exam room supplies and equipment, thereby reducing clutter at the point of care and enhancing patient experience. All exam rooms are accessed from a single circulation spine with elevators and waiting at the center, creating intuitive wayfinding for patients and visitors.
As I write, we are completing a conceptual pricing package for a typical clinic floor developed with significant input from the client’s steering committee and the IPD engineering and construction team. Our next step will be to build a cardboard mockup of all or a portion of the floor for further refinement. Stay tuned for an update this summer.
About the Author
Seena Hassouna
 Seena has a decade of healthcare design and planning experience accumulated during the healthcare building boom in Southern California. He has a keen understanding of the needs of various client having collaborated with for-profit and non-profit health systems. Seena’s ability to work with stakeholders at all levels of a project and translate their needs and goals to a project team and eventually into physical space makes him an integral part of a project team. A well-rounded architect, Seena focuses on the intangible elements of design and space planning that elevate a project from simply being a space or building to becoming a transformative piece of architecture. With a goal of being a fit dad for his two young children, Seena starts his days by exploring New York City with a brisk four mile walk.
Seena has a decade of healthcare design and planning experience accumulated during the healthcare building boom in Southern California. He has a keen understanding of the needs of various client having collaborated with for-profit and non-profit health systems. Seena’s ability to work with stakeholders at all levels of a project and translate their needs and goals to a project team and eventually into physical space makes him an integral part of a project team. A well-rounded architect, Seena focuses on the intangible elements of design and space planning that elevate a project from simply being a space or building to becoming a transformative piece of architecture. With a goal of being a fit dad for his two young children, Seena starts his days by exploring New York City with a brisk four mile walk.

